Interoperability challenges in healthcare AI systems
MODULE 3: PRECISION ONCOTHERAPY
Aug 1, 2025
The interoperability crisis
Healthcare AI has an adoption problem. Despite impressive research results, most AI systems remain isolated research prototypes, never integrated into clinical practice. The reason isn't lack of accuracy or regulatory approval—it's interoperability.
Healthcare institutions run complex digital ecosystems: Electronic Health Records (EHR) systems storing patient data, Picture Archiving and Communication Systems (PACS) managing medical images, Laboratory Information Systems (LIS) tracking test results, Hospital Information Systems (HIS) coordinating operations, pharmacy systems, billing systems, and dozens more specialized applications.
AI systems that can't integrate with these existing workflows are dead on arrival. Clinicians won't manually re-enter data into separate AI platforms. Hospitals won't replace functioning systems just to use new AI tools. And patients suffer when potentially lifesaving technology sits unused because it doesn't fit the workflow.
Interoperability—the ability for different systems to exchange and use information—isn't glamorous. But it's the difference between AI that transforms healthcare and AI that collects dust.
Why healthcare integration is harder than you think
Legacy system complexity: Many hospitals run EHR systems built in the 1990s or early 2000s. These systems weren't designed for AI integration. They use proprietary data formats, closed APIs, and architectures that resist external connectivity. Replacing them would cost hundreds of millions of dollars and disrupt care for years—so integration must work with existing infrastructure.
Data format inconsistency: Healthcare data comes in dozens of formats: HL7 v2, HL7 v3, HL7 FHIR, DICOM for imaging, CDA for documents, X12 for billing, proprietary vendor formats. Each encodes information differently. What one system calls "patient temperature," another might store as "body_temp," "TEMP," or encode within nested XML structures.
Semantic interoperability challenges: Even when systems exchange data successfully, they may interpret it differently. Is "negative" test result good (no disease found) or bad (test failed)? Does "moderate risk" mean 20-30% or 40-60%? Without semantic standards, successful data exchange doesn't guarantee correct interpretation.
Real-time performance requirements: Clinical workflows can't wait. When a radiologist orders an AI analysis of a CT scan, results must return in seconds or minutes, not hours. This demands high-performance APIs, optimized data transfer, and edge computing strategies—not batch processing suitable for research but impractical for clinical use.
Security and privacy constraints: Healthcare data is protected by HIPAA (US), GDPR (EU), and numerous other regulations. Integration architectures must implement encryption, access controls, audit logging, and data governance—without slowing workflows to a crawl. Every API call, data transfer, and system interaction must be secure and compliant.
Multi-institutional coordination: Cancer care typically involves multiple institutions: diagnostic centers, treatment hospitals, research centers, referring physicians. AI systems must exchange data across institutional boundaries while maintaining patient privacy and data sovereignty. This requires federated architectures, not centralized databases.
Standards that enable interoperability
HL7 FHIR (Fast Healthcare Interoperability Resources): The modern standard for health data exchange. FHIR uses RESTful APIs and JSON data formats (familiar to modern developers) to represent clinical concepts: patients, observations, medications, procedures. NoCancer AI uses FHIR to read patient data from EHRs and write AI predictions back into clinical records—making AI recommendations appear seamlessly within existing workflows.
DICOM (Digital Imaging and Communications in Medicine): The universal standard for medical imaging. DICOM defines how to store, transmit, and display images from CT, MRI, mammography, ultrasound, and other modalities. Our imaging AI modules read DICOM files directly from hospital PACS systems, analyze them, and return structured reports in DICOM format—enabling radiologists to view AI findings alongside images in their existing viewers.
IHE (Integrating the Healthcare Enterprise): IHE doesn't create new standards; it profiles existing standards (FHIR, DICOM, HL7) to specify exactly how they should be used for specific workflows. NoCancer AI implements IHE profiles for radiology reporting (IHE RAD), laboratory results (IHE LAB), and cross-enterprise data sharing (IHE XDS)—ensuring plug-and-play compatibility with healthcare IT systems worldwide.
LOINC and SNOMED CT: Standardized medical terminology. LOINC codes laboratory observations (what was measured, in what specimen, using what method). SNOMED CT provides clinical terminology for diagnoses, procedures, and findings. Using standardized codes ensures semantic interoperability—when NoCancer AI reports "elevated CA-125" using standard LOINC codes, every EHR interprets it identically.
OAuth 2.0 and SMART on FHIR: Authorization frameworks enabling secure API access. Rather than storing copies of patient data, NoCancer AI accesses data on-demand with patient consent, using OAuth tokens. SMART on FHIR enables AI applications to launch within EHR interfaces, accessing context (current patient, current encounter) automatically.
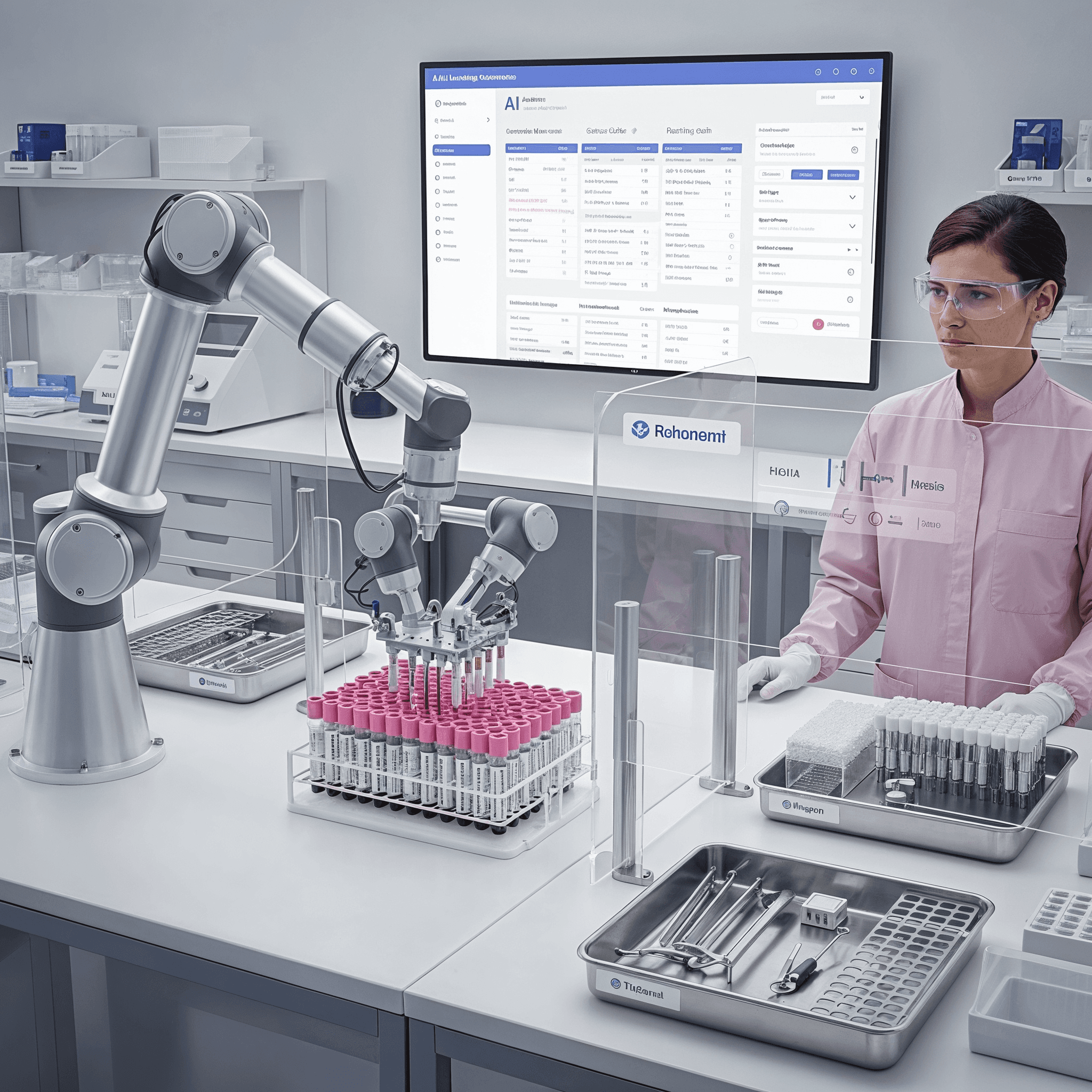
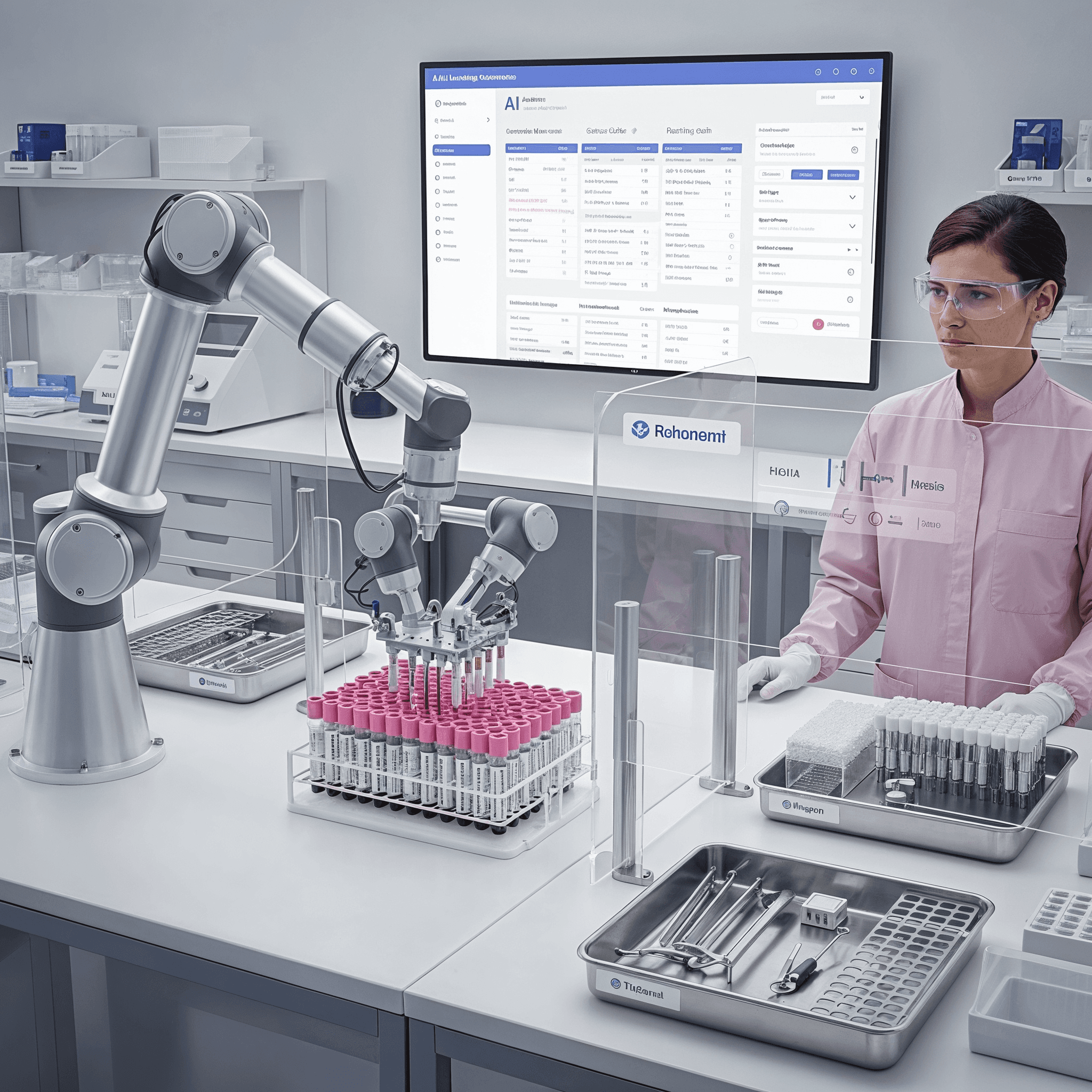
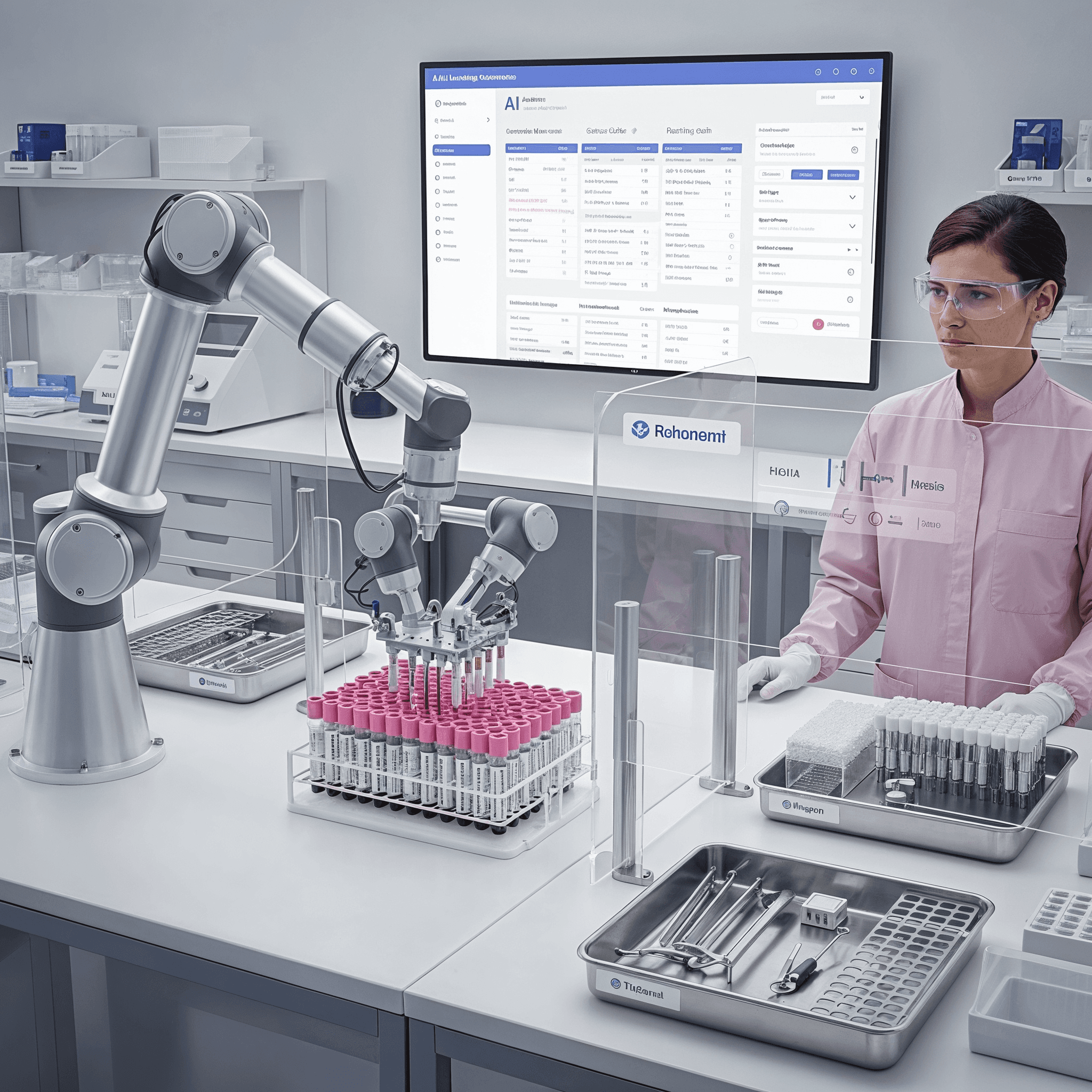
How NoCancer AI implements comprehensive interoperability
Our platform isn't bolted onto clinical systems as an afterthought—it's architected for integration from the ground up.
EHR integration via FHIR:
Read patient demographics, medical history, lab results, medications, allergies directly from institutional EHRs
Write AI predictions as FHIR Observations that appear in patient charts alongside other clinical data
Trigger workflows (like alerting clinicians when cancer risk scores exceed thresholds)
Support SMART on FHIR app architecture enabling launch within Epic, Cerner, and other major EHR systems
PACS integration via DICOM:
Retrieve medical images (mammography, MRI, ultrasound) directly from hospital PACS
Process imaging in-place without requiring separate data copies or exports
Generate DICOM Structured Reports containing AI findings, viewable in standard radiology workstations
Support IHE XDS-I for cross-institutional imaging sharing
LIS/LIMS integration:
Receive laboratory results automatically as they're resulted (proteomics, metabolomics, genomics)
Submit AI requests when new relevant labs complete
Return enhanced interpretations that LIS systems can display alongside raw values
Support HL7 v2 and FHIR for broad laboratory system compatibility
Workflow orchestration:
Clinical Decision Support (CDS) Hooks: AI recommendations appear at appropriate workflow moments (e.g., when ordering screening, reviewing results, planning treatment)
Worklist integration: High-risk patients automatically flagged in radiologist and oncologist worklists
Care coordination: AI predictions shared with multidisciplinary teams through integrated care planning systems
Federated learning for multi-site research:
Train AI models across institutions without centralizing patient data
Differential privacy techniques prevent individual patient re-identification
Blockchain-based consent management gives patients control over data sharing
Real-world integration challenges and solutions
Challenge: Vendor lock-in
Many EHR vendors resist standards-based integration, preferring proprietary connections that lock customers into their ecosystems.
Our solution: NoCancer AI implements both standards-based APIs (preferred) and vendor-specific integration where necessary (Epic MyChart, Cerner APIs). By supporting multiple paths, we maintain interoperability even with resistant vendors—while advocating for open standards adoption.
Challenge: Network performance
Hospital networks often have limited bandwidth, and transferring large imaging datasets (hundreds of megabytes per study) can overwhelm connections.
Our solution: Edge computing architecture runs AI models close to data sources (on-premises or in hospital data centers), minimizing network transfers. Only results—small JSON payloads—cross institutional boundaries.
Challenge: Version fragmentation
Healthcare standards evolve. Some institutions run FHIR R4, others FHIR STU3 or even HL7 v2. Supporting every version is technically demanding.
Our solution: Abstraction layers translate between standard versions. When NoCancer AI integrates with a new institution, configuration specifies which standards that site supports, and our platform automatically adapts communication protocols.
Challenge: Semantic mapping
Different institutions encode the same concept differently. One might record breast density as "dense" vs. "fatty," another uses numeric categories 1-4, a third uses ACR BI-RADS codes.
Our solution: Semantic mapping engine translates institutional conventions to standardized internal representations. Mappings are configurable per institution, and machine learning assists by suggesting mappings based on data patterns.
Challenge: Privacy regulations vary by jurisdiction
GDPR (EU) has different requirements than HIPAA (US) or PIPEDA (Canada). A platform deployed internationally must satisfy all simultaneously.
Our solution: Privacy-by-design architecture implements strictest requirements globally (GDPR), ensuring compliance everywhere. Configurable consent management adapts to local regulations, and federated learning avoids cross-border data transfers that trigger additional restrictions.
The business case for interoperability
Interoperability isn't just technical—it's economic. Healthcare institutions considering AI adoption evaluate:
Total cost of ownership: Systems requiring manual integration (IT staff writing custom code, maintaining interfaces) cost 3-5x more over 5 years than standards-based plug-and-play systems. NoCancer AI's standards-based approach minimizes ongoing integration costs.
Time to deployment: Custom integration projects often take 12-18 months. Standards-based integration can deploy in weeks. Faster deployment means faster return on investment and earlier patient benefit.
Vendor flexibility: Proprietary integration creates lock-in. If you switch EHR vendors, custom integrations break entirely. Standards-based integration is portable—NoCancer AI works with any FHIR-compliant EHR, protecting your investment even if you change vendors.
Scalability: Integrating AI with 5 different EHR systems via custom code requires 5 separate projects. Standards-based integration scales—once configured for FHIR, NoCancer AI integrates with any FHIR system with minimal customization.
The future: Healthcare as a connected ecosystem
Healthcare is shifting from isolated systems to connected ecosystems where data flows seamlessly, AI analyzes continuously, and insights appear at the point of care. This vision requires two things:
Universal standards adoption: Every healthcare system must implement FHIR, DICOM, and IHE profiles. Regulatory pressure (EU's EHDS, US 21st Century Cures Act) is accelerating this transition.
AI-native architectures: Next-generation healthcare systems must be designed for AI from the ground up, with standardized AI model deployment, performance monitoring, and explainability interfaces.
NoCancer AI is built for this future. Our platform isn't just interoperable with today's systems—it's architected for tomorrow's connected healthcare ecosystem.
Because the best AI in the world is worthless if clinicians can't use it. Interoperability makes AI usable. And usable AI saves lives.
FAQ
Answers to your questions
Get quick, clear information about our services, appointments, support, and more
How does NoCancer AI predict cancer 8-10 years early?
Is the temperature-based screening safe?
How do I join the consortium?
What is the EIC Pathfinder Challenge 2025?
How does your AI comply with EU regulations?
FAQ
Answers to your questions
Get quick, clear information about our services, appointments, support, and more
How does NoCancer AI predict cancer 8-10 years early?
Is the temperature-based screening safe?
How do I join the consortium?
What is the EIC Pathfinder Challenge 2025?
How does your AI comply with EU regulations?
FAQ
Answers to your questions
Get quick, clear information about our services, appointments, support, and more
How does NoCancer AI predict cancer 8-10 years early?
Is the temperature-based screening safe?
How do I join the consortium?
What is the EIC Pathfinder Challenge 2025?
How does your AI comply with EU regulations?
Your prevention journey begins with one conversation
Your prevention journey begins with one conversation

Your prevention journey begins with one conversation
Your prevention journey begins with one conversation

Your prevention journey begins with one conversation
Your prevention journey begins with one conversation
